- No category
advertisement
▼
Scroll to page 2
of 20
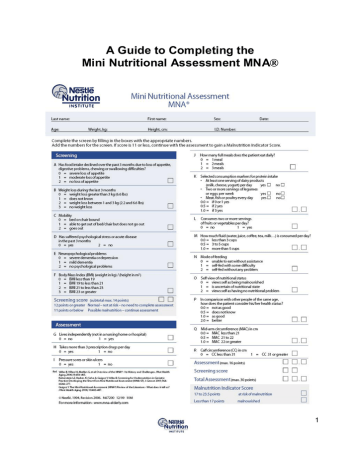
A Guide to Completing the Mini Nutritional Assessment MNA® 1 Mini Nutritional Assessment (MNA®) The MNA® is a screening and assessment tool that can be used to identify elderly patients at risk of malnutrition. The User Guide will assist you in completing the MNA® accurately and consistently. It explains each question and how to assign and interpret the score. Introduction: While the prevalence of malnutrition in the freeliving elderly population is relatively low, the risk of malnutrition increases dramatically in the institutionalized and hospitalized elderly.1 The prevalence of malnutrition is even higher in cognitively impaired elderly individuals and is associated with cognitive decline.2 INSTRUCTIONS TO COMPLETE THE MNA® Before beginning the MNA®, please enter the patient’s information on the top of the form: - Name - Gender - Age - Weight (kg) – To obtain an accurate weight, remove shoes and heavy outer clothing. Use a calibrated and reliable set of scales. If applicable: convert pounds (lbs) to kilograms (1kg = 2.2lbs). - Height (cm) – Measure height without shoes using a stadiometer (height gauge) or, if the patient is bedridden, by knee height or demispan (see Appendices 4 or 5). Convert inches to centimeters (1inch = 2.54cm). - ID number (e.g. hospital number) - Date of screen Patients who are malnourished when admitted to the hospital tend to have longer hospital stays, experience more complications, and have greater risks of morbidity and mortality than those whose nutritional state is normal.3 By identifying patients who are malnourished or at risk of malnutrition either in the hospital or community setting, the MNA® allows clinicians to intervene earlier to provide adequate nutritional support, prevent further deterioration, and improve patient outcomes.4 Mini Nutritional Assessment MNA® The MNA® provides a simple and quick method of identifying elderly patients who are at risk for malnutrition, or who are already malnourished. It identifies the risk of malnutrition before severe changes in weight or serum protein levels occur. The MNA® may be completed at regular intervals in the community and in the hospital or long term care setting. The MNA® was developed by Nestlé and leading international geriatricians and remains one of the few validated screening tools for the elderly. It has been well validated in international studies in a variety of settings5-7 and correlates with morbidity and mortality. 2 Screening (MNA®-SF) Complete the screen by filling in the boxes with the appropriate numbers. Then, add together the numbers to determine the total score of the screen. If the score is 11 or less, continue on with the assessment to determine the Malnutrition Indicator Score. Key Points Ask the patient to answer questions A – E, using the suggestions in the shaded areas. If the patient is unable to answer the question, ask the patient’s caregiver to answer. Using the patient’s medical record or your professional judgment, answer any remaining questions. A. Has food intake declined over the past three months due to loss of appetite, digestive problems, chewing or swallowing difficulties? Score 0 = Severe decrease in food intake 1 = Moderate decrease in food intake 2 = No decrease in food intake Ask patient ð “Have you eaten less than normal over the past three months?” ð If so, “is this because of lack of appetite, chewing, or swallowing difficulties?” ð If yes, “have you eaten much less than before or only a little less?” ð If this is a re-assessment, then rephrase the question: ð “Has the amount of food you have eaten changed since your last assessment?” 3 B. Involuntary weight loss during the last 3 months? Score 0 = Weight loss greater than 3 kg (6.6 pounds) 1 = Does not know 2 = Weight loss between 1 and 3 kg (2.2 and 6.6 pounds) 3 = No weight loss Ask patient / medical record (if long term or residential care) ð “Have you lost any weight without trying over the last 3 months?” ð “Has your waistband gotten looser?” ð “How much weight do you think you have lost? More or less than 3 kg (or 6 pounds)?” Though weight loss in the overweight elderly may be appropriate, it may also be due to malnutrition. When the weight loss question is removed, the MNA® loses its sensitivity, so it is important to ask about weight loss even in the overweight. C. Mobility? Score 0 = Bed or chair bound 1 = Able to get out of bed/chair, but does not go out 2 = Goes out Ask patient / Patient’s medical record / Information from caregiver ð “Are you presently able to get out of the bed / chair?” ð “Are you able to get out of the house or go outdoors on your own? 4 D. Has the patient suffered psychological stress or acute disease in the past three months? Score 0 = Yes 1 = No Ask patient / Patient medical record / Professional judgment ð “Have you suffered a bereavement recently?” ð “Have you recently moved your home? ð “Have you been sick recently?” E. Neuropsychological problems? Score 0 = Severe dementia or depression 1 = Mild depression 2 = No psychological problems Review patient medical record / Professional judgment / Ask nursing staff or caregiver The patient’s caregiver, nursing staff or medical record can provide information about the severity of the patient’s neuropsychological problems (dementia). If a patient cannot respond (i.e. one with dementia) or is severely confused, ask the patient’s personal or professional caregiver to answer the following questions or check the patient’s answers for accuracy (Questions A, B, C, D, G, J, K, L, M, O, P). 5 F. Body mass index (BMI)? (weight in kg / height in m2) Score 0 = BMI less than 19 1 = BMI 19 to less than 21 2 = BMI 21 to less than 23 3 = BMI 23 or greater Determining BMI BMI is used as an indicator of appropriate weight for height. BMI is calculated by dividing the weight in kg by the height in m2 (Appendix 1). BMI = weight (kg) height (m2) Before determining BMI, record the patients’ weight and height on the MNA® form. 1. Convert subject’s weight to metric using formula 1kg = 2.2lbs Convert subject’s height to metric using formula 1inch = 2.54cm 2. If height has not been measured, please measure using a stadiometer or height gauge (Refer to Appendix 3). 3. If the patient is unable to stand, measure height using indirect methods such as measuring demi-span (half arm span) or knee height (See Appendices 4 and 5). If height cannot be measured either directly or by indirect methods, use a verbal or historical height to calculate a BMI. Verbal height will be the least accurate, especially for bedridden patients and patients who have lost height over the years. 4. Using the BMI chart provided (Appendix 1), locate the patient’s height and weight and determine the BMI. It is essential that a BMI is included in the MNA® – without it the tool is not valid. 5. Fill in the appropriate box on the MNA® form to represent the BMI of the patient. 6. To determine BMI for a patient with an amputation, see Appendix 2. The screening section of the questionnaire is now complete. Add the numbers to obtain the screening score. A score of 12 points or greater indicates: Patient is not at nutrition risk. There is no need to complete the rest of the questionnaire. Rescreen at regular intervals. A score of 11 points or less indicates: Patient may be at risk for malnutrition. Please complete the full MNA® assessment by answering questions G – R. 6 Assessment (MNA®) G. Lives independently (not in a nursing home)?) Score 0 = No 1 = Yes Ask patient This question refers to the normal living conditions of the individual. Its purpose is to determine if the person is usually dependent on others for care. For example, if the patient is in the hospital because of an accident or acute illness, where does the patient normally live? ð “Do you normally live in your own home, or in an assisted living, residential setting, or nursing home?” H. Takes more than 3 prescription drugs per day? Score 0 = Yes 1 = No Ask patient / Patient medical record Check the patient’s medication record / ask nursing staff / ask doctor / ask patient I. Pressure sores or skin ulcers? Score 0 = Yes 1 = No Ask patient / Patient’s medical record ð “Do you have bed sores?” Check the patient’s medical record for documentation of pressure wounds or skin ulcers, or ask the caregiver / nursing staff / doctor for details, or examine the patient if information is not available in the medical record. 7 J. How many full meals does the patient eat daily? Score 0 = 1 meal 1 = 2 meals 3 = 3 meals Ask patient / Check food intake record if necessary ð “Do you normally eat breakfast, lunch and dinner?” ð “How many meals a day do you eat?” A full meal is defined as eating more than 2 items or dishes when the patient sits down to eat. For example, eating potatoes, vegetable, and meat is considered a full meal; or eating an egg, bread, and fruit is considered a full meal. K. Selected consumption markers for protein intake ð At least one serving of dairy products per day? ð Two or more servings of legumes or eggs per week? ð Meat, fish or poultry every day? Yes ¨ No ¨ Yes ¨ No ¨ Yes ¨ No ¨ 0.0 = if 0 or 1 Yes answer(s) 0.5 = if 2 Yes answers 1.0 = if 3 Yes answers Ask the patient or nursing staff, or check the completed food intake record ð “Do you consume any dairy products (a glass of milk / cheese in a sandwich / cup of yogurt / can of high protein supplement) every day?” ð ”Do you eat beans/eggs? How often do you eat them?” ð “Do you eat meat, fish or chicken every day?” 8 L. Consumes two or more servings of fruits or vegetables per day? Score 0 = No 1 = Yes Ask the patient / check the completed food intake record if necessary ð “Do you eat fruits and vegetables?” ð ”How many portions do you have each day?” A portion can be classified as: One piece of fruit (apple, banana, orange, etc.) One medium cup of fruit or vegetable juice One cup of raw or cooked vegetables M. How much fluid (water, juice, coffee, tea, milk) is consumed per day? Score 0.0 = Less than 3 cups 0.5 = 3 to 5 cups 1.0 = More than 5 cups Ask patient ð “How many cups of tea or coffee do you normally drink during the day?” ð ”Do you drink any water, milk or fruit juice? What size cup do you usually use? A cup is considered 200 – 240ml or 7-8oz. 9 N. Mode of Feeding? Score 0 = Unable to eat without assistance * 1 = Feeds self with some difficulty ** 2 = Feeds self without any problems Ask patient / Patient medical record/ information from caregiver ð “Are you able to feed yourself?” / “Can the patient feed himself/herself?” ð ”Do you need help to eat?” / “Do you help the patient to eat?” ð “Do you need help setting up your meals (opening containers, buttering bread, or cutting meats)?” *Patients who must be fed or need help holding the fork would score 0. **Patients who need help setting up meals (opening containers, buttering bread, or cutting meats), but are able to feed themselves would score 1 point. Pay particular attention to potential causes of malnutrition that need to be addressed to avoid malnutrition (e.g. dental problems, need for adaptive feeding devices to support eating). O. Self-View of Nutritional Status Score 0 = Views self as being malnourished 1 = Is uncertain of nutritional state 2 = Views self as having no nutritional problems Ask patient ð “How would you describe your nutritional state?” Then prompt ”Poorly nourished?” “Uncertain?” “No problems?” The answer to this question depends upon the patient’s state of mind. If you think the patient is not capable of answering the question, ask the caregiver / nursing staff for their opinion. 10 P. In comparison with other people of the same age, how does the patient consider his/her health status? Score 0.0 = Not as good 0.5 = Does not know 1.0 = As good 2.0 = Better Ask patient ð “How would you describe your state of health compared to others your age?” Then prompt: ”Not as good as others of your age?” “Not sure?" “As good as others of your age?" “Better?” Again, the answer will depend upon the state of mind of the person answering the question. Q. Mid-arm circumference (MAC) in cm Score 0.0 = MAC less than 21 0.5 = MAC 21 to 22 1.0 = MAC 22 or greater Measure the mid-arm circumference in cm as described in Appendix 6. 11 R. Calf circumference (CC) in cm Score 0 = CC less than 31 1 = CC 31 or greater Calf circumference should be measured in cm as described in appendix 7. Measure the calf at the widest area. Take additional measurements above and below the widest point to ensure that the first measurement was the largest. Final Score ð Total the points from the assessment section of the MNA® (maximum 16 points). ð Add the assessment and screening scores together to get the total Malnutrition Indicator Score (Maximum 30 points). ð Check the appropriate box indicator. ð If the score is greater than 23.5 points, the patient is in a normal state of nutrition and no further action is required. ð If the score is less than 23.5 points, refer the patient to a dietitian or nutrition specialist for nutrition intervention. Until a dietitian is available, give the patient / caregiver some advice on how to improve nutritional intake such as: ð Increase intake of energy/protein dense foods (e.g. puddings, milkshakes, etc). ð Supplement food intake with additional snacks and milk. ð If diet alone does not improve the patient’s nutritional intake, the patient may need oral nutritional supplements. ð Ensure adequate fluid intake; 6-8 cups / glasses per day Follow-Up ð Re-screen all patients every three months. ð Please refer results of assessments & re-assessments to dietitian/doctor and record in medical record. 12 Appendices Appendix 1 BODY MASS INDEX TABLE Source: Adapted from Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. National Institute of Health, National Heart Lung and Blood Institute 13 Appendix 2 DETERMINING BMI FOR AMPUTEES ðTo determine the BMI for amputees, first determine the patient’s estimated weight including the weight of the missing body part.8,9 − Use a standard reference (see table) to determine the proportion of body weight contributed by an individual body part. − Multiple patient’s current weight by the percent of body weight of the missing body part to determine estimated weight of missing part. − Add the estimated weight of the missing body part to patient’s current weight to determine estimated weight prior to amputation. ð Divide estimated weight by estimated body height2 to determine BMI. WEIGHT OF SELECTED BODY COMPONENTS It is necessary to account for the missing body component(s) when estimating IBW. Table Percent of Body Weight Contributed by Specific Body Parts Body Part Trunk w/o limbs Percentage 50.0 Hand Forearm with hand 0.7 2.3 Forearm without hand Upper arm Entire arm Foot Lower leg with foot Lower leg without foot Thigh Entire leg 1.6 2.7 5.0 1.5 5.9 4.4 10.1 16.0 References cited: Malone A. Anthropometric Assessment. In Charney P, Malone E, eds. ADA Pocket Guide to Nutrition Assessment. Chicago, IL: American Dietetic Association; 2004:142-152. Osterkamp LK. Current perspective on assessment of human body proportions of relevance to amputees. J Am Diet Assoc. 1995;95:215-218. Example: 80 year old man, amputation of the left lower leg, 1.72 m, 58 kg 1. Estimate body weight: Current body weight + Proportion for the missing leg 58 (kg) + [58 (kg) x 0.059] = 61.4 kg 2. Calculate BMI: Estimated body weight / body height (m) 2 61.4 / 1.72 x 1.72 = 20.8 3. Calculate energy intake: ð Recommended energy intake – 5.9% ð Empirical formula (30 kcal/kg/day): 30 kcal/kg/d X [61.4 kg – (61.4 x 0.059)] = 1,832 kcal/day Conclusion: Corrected BMI is 21, and estimated energy intake is 1,800 – 1,900 kcal/d 14 Appendix 3 MEASURING HEIGHT USING A STADIOMETER Accessed at: http://www.ktl.fi/publications/ehrm/product2/part_ iii5.htm 1. Ensure the floor surface is even and firm. 2. Have subject remove shoes and stand up straight with heels together, and with heels, buttocks and shoulders pressed against the stadiometer. 3. Arms should hang freely with palms facing thighs. 4. Take the measurement with the subject standing tall, looking straight ahead with the head uprights and not tilted backwards. 5. Make sure the subjects heels stay flat on the floor. 6. Lower the measure on the stadiometer until it makes contact with the top of the head. 7. Record standing height to the nearest centimeter. 15 Appendix 4 MEASUREMENT OF DEMISPAN ð Demispan (half-arm span) is the distance from the midline at the sternal notch to the tip of the middle finger Height is then calculated from a standard formula.10 1. Locate and mark the edge of the right collar bone (in the sternal notch) with the pen. 2. Ask the patient to place the left arm in a horizontal position. 3. Check that the patient’s arm is horizontal and in line with shoulders. 4. Using the tape measure, measure distance from mark on the midline at the sternal notch to the tip of the middle finger. 5. Check that arm is flat and wrist is straight. 6. Take reading in cm. Calculate height from the formula below: Females Height in cm = (1.35 x demispan in cm) + 60.1 Males Height in cm = (1.40 x demispan in cm) + 57.8 Source: http://www.rxkinetics.com/height_estimate.htm l . Accessed December 12, 2006. 16 Appendix 5 MEASUREMENT OF KNEE HEIGHT ð Knee height is one method to determine statue in the bed- or chair-bound patient and is measured using a sliding knee height caliper. The subject must be able to bend the knee and the ankle to 90 degree angles. 1. Have the subject bend the knee and ankle of one leg at a 90 degree angle while lying supine or sitting on a table with legs hanging off the side of the table. 2. Place the fixed blade of the knee caliper under the heel of the foot in line with the ankle bone. Place the fixed blade of the caliper on the anterior surface of the thigh about 3.0 cm above the patella. 3. Be sure the shaft of the caliper is in line with and parallel to the long bone in the lower leg (tibia) and is over the ankle bone (lateral malleolus). Apply pressure to compress the tissue. Record the measurement to the nearest 0.1 cm. 4. Take two measurements in immediate auccession. They should agree within 0.5 cm. Use the average of these two measurements and the person's chronological age in the Country and ethnic group specific equations in the following table. 5. The value calculated from the selected equation is an estimate of the person's true stature. The 95 percent confidence for this estimate is plus and minus twice the SEE value for each equation. Source: http://www.rxkinetics.com/height_estimate.htm l . Accessed December 12, 2006. 17 Using population-specific formula, calculate height from standard formula: Gender and ethnic group Equation Non-Hispanic white men (U.S.)11 [SEE = 3.74 cm] Stature (cm) = 78.31+(1.94 x knee height) – (0.14 x age) Non-Hispanic black men (U.S.)11 [SEE = 3.80 cm] Stature (cm) = 79.69+(1.85 x knee height) – (0.14 x age) Mexican-American men (U.S.)11 [SEE = 3.68 cm] Stature (cm) = 82.77+(1.83 x knee height) – (0.16 x age) Non-Hispanic white women (U.S.)11 [SEE = 3.98 cm] Stature (cm) = 82.21+(1.85 x knee height) – (0.21 x age) Non-Hispanic black women (U.S.)11 [SEE = 3.82 cm] Stature (cm) = 89.58+(1.61 x knee height) – (0.17 x age) Mexican-American women (U.S.)11 [SEE = 3.77 cm] Stature (cm ) = 84.25+(1.82 x knee height) – (0.26 x age) Taiwanese men12 [SEE = 3.86 cm] Stature (cm) = 85.10 + (1.73 x knee height) – (0.11 x age) Taiwanese women12 [SEE = 3.79 cm] Stature (cm) = 91.45 + (1.53 x knee height) – (0.16 x age) Elderly Italian men13 [SEE = 4.3 cm] Stature (cm) = 94.87 – (1.58 x knee height) – (0.23 x age) +4.8 Elderly Italian women13 [SEE = 4.3 cm] Stature (cm) = 94.87 + (1.58 x knee height)– (0.23 x age) French men14 [SEE = 3.8 cm] Stature (cm) = 74.7 + (2.07 x knee height) – (-0.21 x age) French women14 [SEE = 3.5 cm] Stature (cm) = 67.00 + (2.2 x knee height) – (0.25 x age) Mexican Men15 [SEE = 3.31 cm] Stature (cm) = 52.6 + (2.17 x knee height) Mexican Women15 [SEE = 2.99 cm] Stature (cm) = 73.70 + (1.99 x knee height) – (0.23 x age) Filipino Men16 Stature (cm) = 96.50 + (1.38 x knee height) – (0.08 x age) 16 Stature (cm) = 89.63 + (1.53 x knee height) – (0.17 x age) 17 Malaysian men [SEE = 3.51 cm] Stature (cm) = (1.924 x knee height) + 69.38 Malaysian women17 [SEE = 3.40] Stature (cm) = (2.225 x knee height) + 50.25 Filipino Women 18 Appendix 6. MEASURING MID ARM CIRCUMFERENCE 1. Ask the patient to bend their non-dominant arm at the elbow at a right angle with the palm up. 2. Measure the distance between the acromial surface of the scapula (bony protrusion surface of upper shoulder) and the olecranon process of the elbow (bony point of the elbow) on the back of the arm. 3. Mark the mid-point between the two with the pen. 4. Ask the patient to let the arm hang loosely by his/her side. 5. Position the tape at the mid-point on the upper arm and tighten snugly. Avoid pinching or causing indentation. 6. Record measurement in cm. 7. If MAC is less than 21, score = 0. If MAC is 21-22, score = 0.5. If MAC is 22 or greater, score = 1.0. Source: Moore MC Pocket Guide to Nutrition and Diet Therapy. 1993 Source: PEN Group. A pocket guide to clinical nutrition: Assessment of nutritional status. British Dietetic Association. 1997 Appendix 7 MEASURING CALF CIRCUMFERENCE 1. The subject should be sitting with the left hanging loosely or standing with their weight evenly distributed on both feet. 2. Ask the patient to roll up their trouser leg to uncover the calf 3. Wrap the tape around the calf at the widest part and note the measurement. 4. Take additional measurements above and below the point to ensure that the first measurement was the largest. 5. An accurate measurement can only be obtained if the tape is at a right angle to the length of the calf, and should be recorded to the nearest 0.1 cm. 19 References 1. Guigoz Y, Vellas B. Garry PJ. Assessing the nutritional status of the elderly: The Mini Nutritional Assessment as part of the geriatric evaluation. Nutr Rev 1996;54:S59-S65. 2. Fallon C, Bruce I, Eustace A, et al. Nutritional status of community dwelling subjects attending a memory clinic. J Nutr Health Aging 2002;6(Supp):21. 3. Kagansky N, Berner Y, Koren-Morag N, Perelman L, Knobler H, Levy S. Poor nutritional habits are predictors of poor outcomes in very old hospitalized patients. Am J Clin Nutr 2005;82:784791. 4. Vellas B, Villars H, Abellan G et al. Overview of the MNA® – It’s history and challenges. J Nutr Health Aging 2006;10:455-465. 5. Guigoz Y, Vellas J, Garry P (1994). Mini Nutritional Assessment: A practical assessment tool for grading the nutritional state of elderly patients. Facts Res Gerontol 4 (supp. 2):15-59. 6. Guigoz Y. The Mini-Nutritional Assessment (MNA®) review of the literature – what does it tell us? J Nutr Health Aging 2006;10:465-487. 7. Murphy MC, Brooks CN, New SA, Lumbers ML. The use of the Mini Nutritional Assessment (MNA) tool in elderly orthopaedic patients. Eur J Clin Nutr 2000;54:555-562. 8. Malone A. Anthropometric Assessment. In Charney P, Malone E, eds. ADA Pocket Guide to Nutrition Assessment. Chicago, IL: American Dietetic Association; 2004:142-152. 9. Osterkamp LK. Current perspective on assessment of human body proportions of relevance to amputees. J Am Diet Assoc. 1995;95:215-218. 10. HIckson M, Frost G. A comparison of three methods for estimating height in the acutely ill elderly population. J Hum Nutr Diet 2003;6:1-3. 11. Chumlea WC, Guo SS, Wholihan K, Cockram D, Kuczmarski RJ, Johnson CL. Stature prediction equations for elderly non-Hispanic white, non-Hispanic black, and Mexican-American persons developed from NHANES III data. J Am Diet Assoc 1998;98:137-142. 12. Cheng HS, See LC, Sheih. Estimating stature from knee height for adults in Taiwan. Chang Gung Med J. 2001;24:547-556. 13. Donini LM, de Felice MR, De Bernardini L, et al. Prediction of stature in the Italian elderly. J Nutr Health Aging. 2004;8:386-388. 14. Guo SS, Wu X, Vellas B, Guigoz Y, Chumlea WC. Prediction of stature in the French elderly. Age & Nutr. 1994;5:169-173. 15. Mendoz-Nunez VM, Sanchez-Rodriguez MA, Cervantes-Sandoval A, et al. Equations for predicting height for elderly Mexican-Americans are not applicable for elderly Mexicans. Am J Hum Biol 2002;14:351-355. 16. Tanchoco CC, Duante CA, Lopez ES. Arm span and knee height as proxy indicators for height. J Nutritionist-Dietitians’ Assoc Philippines 2001;15:84-90. 17. Shahar S, Pooy NS. Predictive equations for estimation of statue in Malaysian elderly people. Asia Pac J Clin Nutr. 2003:12(1):80-84. 20
advertisement
* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
